Can a Neurodisability Nursing Framework Strengthen Learning Disability Nursing: Reflections from an RCN/Oxleas Event
Jonathan Beebee, RNLD, CEO & Nurse Consultant for PBS4
On 6th February the RCN and Oxleas NHS Trust co-hosted an event about promoting learning disability nursing. A large drive for this event has been an acceleration in recent years on the debate about whether the field of registration should be renamed. This article is a personal reflection on this topic following this event. I must be clear, this article does not represent an agreed position of the Royal College of Nursing – I am intentionally sharing this as CEO and Nurse Consultant of PBS4 to ensure separation. The RCN does not currently hold a position on whether the field of Registered Nurses in Learning Disabilities (RNLD) registration should change. The discussion explored at this event arose because RNLDs themselves have asked for space to consider the future shape and sustainability of the profession.
I originally shared my views on this in November 2023. I have carefully listened to concerns regarding what was said then and my vision for how this could materialise has changed in response to these concerns. However, I have not publicly shared my views since then, so I intend to outline my vision for this here. Perhaps you have strong views on this already, and perhaps you have formed views based upon what has previously been expressed. However, please read this with an open mind to accurately consider what is being proposed here.
“Nobody knows what we do”
These are the words I hear from learning disability nurses at least once per week. Professor Sara Ryan is currently articulating this really well when she describes “the wise” (those whose lives are embedded in the realities people with learning disabilities face everyday), and “the collective” (the rest of the population who continuously remain oblivious to the complexities of health needs and the daily challenges people face). We need to be real about this, the general public just don’t get it, and if they don’t get that is it any surprise there is limited understanding of why there is a dedicated field of nursing registration for learning disabilities with the Nursing & Midwifery Council (NMC)?
There are many possible explanations about why the realities people with learning disabilities face continue to be misunderstood. Our language has changed over time to reduce associations with diagnostic terms that became offensive, and there is confusion around learning disabilities and difficulties. The primary concept of learning disabilities and the support people need has moved from a medical model to a social model. In recent times, policy has grouped learning disabilities with autism – this began with Valuing People (DH, 2001) where we began saying people with learning disabilities and/or autism to avoid people with autism who didn’t quite meet learning disability criteria falling through the gaps – this has now progressed to policy typically taking a “learning disability and autism” position, a growth since the pandemic of neurodivergence awareness and collectiveness, and presently the neurodivergent voice (without learning disability) overshadowing the voices of people with learning disability. We have also had a warmly welcomed growth in co-production and lived experience, but the lived experience that the public and policy makers see can be very different to the lived experiences of the people learning disability nurses see day-to-day due to their abilities to engage in these initiatives.
This all contributes to the work learning disability nurses do being unrecognised and misunderstood. It leads to challenges attracting students to this field of nursing. It also challenges service providers, commissioners, and policy makers in designing services for those who need them most.
Learning disability nursing roles are essential
Before I go any further, I need to be absolutely clear that my view is that the role of “learning disability nurses”, i.e. specific jobs that are dedicated to providing skilled nursing support exclusively to people with learning disabilities remain essential. We save lives. We provide interventions that sustain family lives. We prevent secure hospital admission and support effective discharges. We prevent injury and contact with the criminal justice system. Essentially, we identify health needs when they can be difficult to identify and ensure access to health and social care for people when they need it. We also provide interventions that promote independence for people, no mater how small a step this is towards independence, every tiny step is recognised, celebrated, and built upon.
Changes to our field of registration does not mean a change to what services are commissioned or to “learning disability nursing” jobs. Any learning disability nurse will tell you how busy they are, how the complexity of their work continues to increase, and how vital their work is. This event was held for RNLDs and students in London and the South East. This is significant as the South East is the first region in England where there is no HEI offering pre-registration learning disability nurse training except for the Open University. NHS England predict that if the current rate of decline in student numbers and university options continues then pre-registration learning disability nursing training will not be sustainable in England from 2028.
So what would a future with no new entrants to the NMC register mean? The reality is the field of registration would fade away. Learning disability nursing jobs would likely continue, but they would be appointed to Registered Nurses from other fields. We are seeing this already with learning disability nursing jobs being advertised for RNLD/RNMH. Where RNMHs are filling these positions we are not seeing these roles suddenly working with people with mental health needs for people who don’t have a learning disability. This demonstrates that registration title does not dictate roles in response to concerns that broadening the scope of registration would mean learning disability roles would see a broader range of people. However, we have seen roles where this has happened, such as acute learning disability and autism liaison nursing roles, so safeguards would need to be in place.
Learning disability nursing jobs are not the problem here – it is our field of registration that is the problem. Our registration with the NMC is not our roles, it is our ticket to say we are eligible for roles. It is vital that we separate the two out to continue a specific field of registration for learning disability nursing jobs and there are numerous sources of evidence that quality reduces when RNLDs are substituted by other health professionals for learning disability nursing roles. This is about protecting learning disability nursing jobs, not diluting them.
A framework for Registered Nurses in Neurodisabilities
The vision presented here is about strategically broadening the scope of practice that this point of registration covers. It is broadening the scope to neuroscience practice, which is already largely covered in RNLDs training and practice and our role in supporting neurodivergence.
At present, the title of RNLD poses barriers to this. I hear regularly from RNLDs who are denied roles in neurology (e.g. epilepsy services) as their professional registration implies they can only support people with learning disabilities and there are misconceptions that they do not have the nursing skills required for these roles. RNLDs can also face barriers and challenges in services supporting neurodivergent people who can take objection that being supported by a RNLD implies that they have a learning disability. This strategic repositioning of the field of registration instantly dispels these challenges.
Therefore, the change being proposed here is changing the point of registration to be Registered Nurse in Neurodisabilities.
‘Neurodisability as an umbrella term for conditions associated with impairment of the brain and/or neuromuscular system, resulting in functional limitations that affect movement, cognition, communication, or behaviour, and often require long-term support.’
Morris, C., & Janssens, A. (2022).
The diagram below illustrates how learning disability nursing sits as a defined, protected specialty within a broader and more sustainable neurodisability registration.
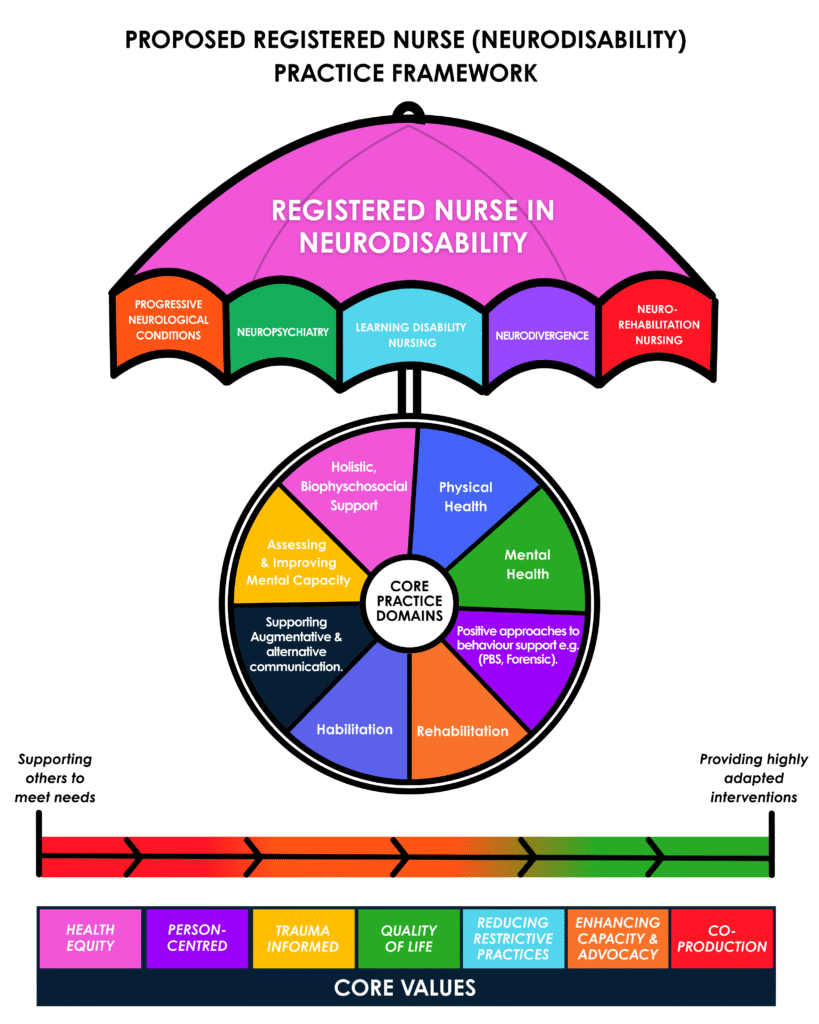
This image depicts the vision for a framework for Registered Nurses in Neurodisabilities. Learning Disability Nursing remains a core, specific and distinct field of practice under this registration – similar to how cancer nursing practice is a field of practice for Registered Nurses for Adults. It opens doors for us that many RNLDs face as closed presently in other areas of neuroscience practice. The core domains we have are equally relevant to learning disabilities as they are to neuro-rehabilitation or any other area. Our scope of practice ranges from enabling other services to meet peoples need to providing our own specific interventions. And there are core values that underpin what we do.
The stark reality is that the job opportunities available for “learning disability nurses” has significantly declined since 2009. Repositioning the point of registration in this way broadens the career opportunities for Registered Nurses, which attracts more students and creates more student placements, and cements a professional registration for learning disability nursing jobs and learning disability nurses to advocate for people with learning disabilities.
It is also important to note that “neurodisability” is already a recognised term and is growing in its use, particularly in children’s services. This is not new terminology. It is language that is being used where “learning disability” is already being recognised as not enough to get people and families the support they need. I invite readers to conduct an internet search of “neurodisability services” and look at the services that are already out there. I know from my conversations with learning disability nurses that they see this title as pulling us closer towards neurodivergence. I also know from my conversations with “the collective” that this is not seen as that, but seen instead as pulling us closer to neuroscience.
This is not about shifting focus away from people with learning disabilities. It is about ensuring that learning disability nursing is professionally positioned within the same systems that shape neurological and long-term condition care more broadly—systems that already have significant impact on the lives of people with learning disabilities.
This Is About Reframing Nursing at Point of Registration, Not Reframing People
A potential risk of this is moving learning disability nursing under a neurodisability, and therefore neuroscience, umbrella leads to a medicalisation of people with learning disabilities. Could the same not be argued for the existence of learning disability “nurses”? This is not about repositioning people with learning disabilities, it is about ensuring they have competent nursing support when they need it. People with learning disabilities do not need reframing, and this is not suggesting we change how we refer to people with learning disabilities – people do not need reframing and it is up to them what identity they choose to use.
What does require attention is how learning disability nursing itself is structured, protected, and understood within health and care systems. The question being explored is how nursing practice can be sustainably organised in a way that safeguards specialist roles, supports workforce development, creates job and student opportunities, and enables effective interface with increasingly complex health systems without losing its values or purpose.
This matters not because people need to be understood differently, but because nursing needs to be intelligible within the systems that allocate resources, design services, and plan workforces. If learning disability nursing is to be recognised, protected, and adequately resourced, it must be professionally legible within those systems.
Leaning into neuroscience in this context is not about changing how people are seen; it is about strengthening how nursing is positioned.
The voices of people with learning disabilities are important in this conversation. However, first we need clarity about what we want to hear their opinions on. If the profession has no desire to change then there is no conversation to be had. If there is desire for change we need to engage people with learning disabilities in this conversation. We may also need to consult with others who may come under the neurodisability umbrella to ensure all affected are consulted.
Why “Neurodisability”?
Throughout this conversation I have listened to a variety of other suggestions for different titles that could be applied to modernise “Registered Nurses in Learning Disabilities.
Registered Nurses in Intellectual Disabilities has been suggested. This would bring the UK language in line with international terminology. This may help the public understand the difference between learning disability, learning difficulty, and neurodivergence. However, it would not increase the career opportunities for the profession. Without career expansion it is unlikely to attract more students, and the narratives of “a dying profession” remain. There are also growing views around why in the 21st century we are describing people as being disabled in academic achievements of learning and intellect.
Registered Nurses in Neurodevelopment has also been suggested. This has also been considered by the Royal College of Psychiatrists in renaming Learning Disability Psychiatrists to Neurodevelopmental Psychiatrists. This however faces the same challenges as “Registered Nurses in Intellectual Disabilities” in that it doesn’t increase job opportunities and therefore may not increase student attraction. It has the added challenge of the “developmental” part implying it relates to children.
Registered Nurses in Neurodivergence is another suggestion. If you have listened to the vocal neurodivergent communities you will hear clear messages that they do not need “fixing” or “treating” and there would likely be strong objection from the neurodivergent community to this. Which leads to the question whether the learning disability community who are able to be part of co-production initiatives feel that having Registered Nurses in Learning Disabilities implies that a learning disability is an illness.
Ending Where We Need to Start
The resistance I have carefully listened to during this event and over the last few years is not resistance to change for its own sake. It is resistance born from a long history of learning disability nursing feeling marginalised, misunderstood, and vulnerable to erosion.
That resistance deserves respect. But it should not prevent us from asking difficult questions about how the profession survives and thrives over the next 20–30 years.
If we do nothing, the risks are already visible. If we think boldly—but carefully—we may yet secure a future in which learning disability nursing is not diluted or displaced, but strengthened by being clearly, confidently, and sustainably positioned within neurodisability nursing.
RNLDs are united that the outlook is bleak and something needs to change. The current impression is that RNLDs are divided by this debate, and that division is leading to inaction. I don’t think we have time for further inaction. If RNLDs support this change we need to hear your voices. If you think I am barking up the wrong tree, then I need to hear that too so I can cease efforts on this. The only way I will know is by hearing your voice; I therefore invite RNLDs, student learning disability nurses, and anyone else who cares about the future of the field of Registered Nurses in Learning Disabilities to complete this survey to share their thoughts. This survey will close on 13th March 2026. Please complete it yourself and share with others to encourage their completion. Opinions on changing the field of Registered Nurses in Learning Disabilities – Fill out form
We need RNLDs to be loud right now. If the profession is silent it writes its own ending. Please blog yourself on this topic, discuss it with your colleagues, and consider other ways of progressing this conversation.
Written by: Jonathan Beebee, RNLD, CEO & Nurse Consultant for PBS4